
Diseases of the genitourinary system in men are difficult to treat and have a recurring nature. Prostate pathologies affect hormonal levels, emotional state, erectile and genitourinary function.
The treatment of prostatitis in men is complicated by the fact that in the early stages of development, disorders practically do not manifest themselves symptomatically. The first signs appear when the disease is advanced. Early diagnosis and an adequately prescribed course of treatment are the key to a favorable prognosis in the fight against pathology.
What is prostatitis
With a few exceptions, the term "prostatitis" refers to chronic or acute inflammation of the prostate gland. Manifestations of prostatitis in men are similar to the symptoms of other pathologies of the genitourinary system. The process leads to blockage of the glandular tissues and the appearance of the following disorders:
- Dysuric disorders.
- Decreased sexual desire.
- Erectile dysfunction.
- Pain syndrome.
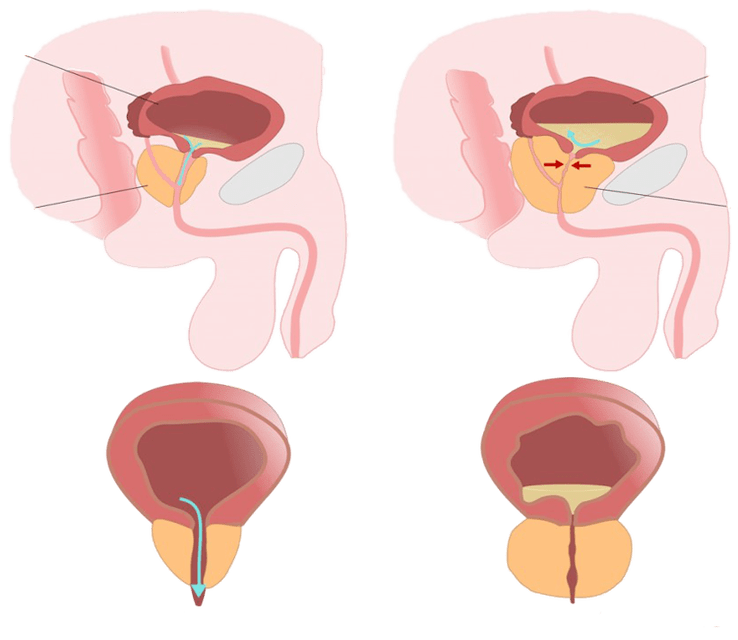
The disease provokes the formation of adhesions and scars. Metabolism and blood circulation in the tissues gradually deteriorate. Irreversible changes occur that can only be corrected by surgery. There are several types of disorders depending on the etiology and stage of development.
Categories prostatitis
Inflammation of the prostate gland matures against the background of congestion in the pelvic region. The process quickly becomes chronic. The favorable time for treatment is the early stage of the disease.
Medical reference books describe 4 types of disease with characteristic symptoms and manifestations:
- Category I—
Acute prostatitis. The catalyst is an infection that has entered the tissue, injury and hypothermia of the gland. The inflammation occurs suddenly and lasts 3-4 days. Without the necessary therapy, it becomes chronic. Manifestations:- heat,
- fever,
- pain in the pelvis and lumbar region,
- intoxication of the body.
- II category—
Chronic bacterial prostatitis. It starts with an aggravation. Cause of appearance: interrupted course of antibiotics, self-medication. The inflammation proceeds in a latent form, without visible manifestations, until the immune system weakens so much that the infection triggers an exacerbation of the disease. Treatment begins with antibiotics and NSAIDs. - III category—
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Disease mutated from acute inflammation of the prostate gland. Disturbances develop slowly, irreversible changes occur, leading to tissue blockage. Stagnant inflammation, in turn, is divided into two subgroups:Category IIIa - Chronic prostatitis/chronic pelvic pain syndrome with signs of inflammation. It is characterized by pronounced manifestations: low fever, rising during an exacerbation to 38-38. 5 °. Characteristic symptoms of male prostatitis: deterioration of erection, hemospermia, prolonged intercourse without orgasm, impaired urination.Category IIIb - Chronic prostatitis/chronic pelvic pain syndrome without signs of inflammation. In this case, the manifestations are diagnosed exclusively with the help of instrumental research methods.
- IV category—
Asymptomatic (symptomless) chronic prostatitis. It is considered a poorly understood disease of unknown etiology. Some leading urologists suggest that the cause of the disease is related to age. There are no symptoms of pathology.
It is difficult to cure prostatitis even at an early stage. In order to achieve a stable remission, it will be necessary to eliminate the causes - catalysts, to deal with the complications and consequences that arise.
Why is prostatitis dangerous?
Inflammation of the prostate gland is a serious pathology that affects men's health. Possible complications and consequences of the disease:

- erectile dysfunction- scars and adhesions, the result of inflammation, obstruct the normal blood flow in the cavernous vessels. At the same time, the prostate's ability to process testosterone deteriorates. Sexual desire decreases. In the acute period, friction and ejaculation cause pain. All of the above causes the erection to deteriorate. In some cases, complete sexual impotence is diagnosed.
- Infertility— chronic inflammation affects not only the prostate, but also spreads to adjacent parts and organs of the genitourinary system. Degenerative disorders are often manifested in the ligament: testicles + glandular tissues. The quality and volume of spermatogenesis deteriorates. Getting pregnant by a man with advanced prostatitis is problematic.
- Development of associated diseases- the inflammation can spread to neighboring organs of the genitourinary system:
- urethral canal,
- bladder,
- kidneys,
- scrotum
- Death— there is a danger of death in purulent disease. If the treatment of acute male prostatitis is not started in a timely manner and purulent formations appear that develop into an abscess, the patient's life is at risk. A ruptured cavity to the rectum leads to general intoxication and can lead to death.
In severe cases, surgery is required. Unlike adenoma or malignant hyperplasia, surgery is prescribed extremely rarely and does not guarantee prevention of recurrence.
Which doctor treats prostatitis
It all depends on the manifestations of the disease. The urologist remains the main one. It is this specialist who deals with pathologies of the male genitourinary system, including inflammation of the prostate. In case of some violations, it will be necessary to involve doctors from another specialty.

Current clinical guidelines indicate the need to promote:
- Psychiatrist— help is needed if pain and other manifestations create a psychological rejection of sexual relations, impotence without physical disorders.
- Immunologist— long-term antibacterial and drug therapy takes a heavy toll on the body. Protective functions and the ability to resist infection are reduced. Some forms of prostatitis begin with autoimmune diseases. In each of these situations, the help of an immunologist will be necessary.
- A surgeon— opening of purulent abscesses, performing TUR, prostatectomy and removal of calcifications is performed by a specialist. A surgeon's help will be needed to remove adhesions in the seminal ducts and restore reproductive function.
Such a number of specialists needed for the complete cure of the patient convincingly proves that it is impossible to cure prostatitis on your own, let alone get rid of complications. Qualified help is required.
How to recognize prostatitis
The insidiousness of the disease lies in the fact that over a long period of time the inflammation develops asymptomatically in a latent form. The first signs of prostatitis are often attributed to: fatigue, radiculitis, diseases of the genitourinary system. The pain stops after taking an analgesic or antispasmodic tablet. But the inflammation of the prostate gland continues until the disorders become global. A person goes to the doctor, where they give him an unpleasant diagnosis.
Still, the most effective way to get rid of prostatitis is early diagnosis and immediate treatment. The chances of a complete cure are about 80%.
To distinguish inflammation from other diseases, several diagnostic tests are performed:
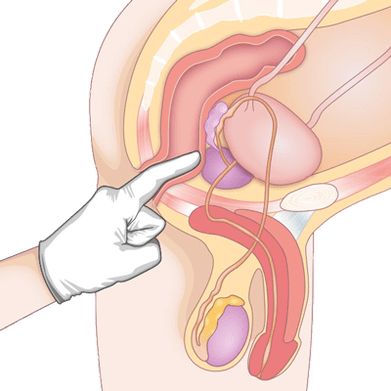
- Rectal method— the doctor examines the structure of the gland by inserting a finger into the anus, which allows all abnormalities and deviations to be identified.
- Ultrasound and TRUS— Ultrasound diagnosis remains the standard of investigation due to its low cost and availability. The monitor shows a loose structure of the gland, which indicates inflammation, it is possible to detect calcifications and other signs of prostatitis.
- Clinical and biochemical tests of blood and urine- indicate the presence of inflammation and also identify an infectious agent.
- spermogram- reduced vitality and speed of spermatozoa, characteristic signs of congestive prostatitis and blockage of glandular tissues. During an infectious disease, bacteria and pathogens are found in the ejaculate.
- MRI and PET-CT- the most reliable diagnostic methods. Due to the high cost, the test is prescribed only if the results of previous tests are unclear, as well as when cancer is suspected.
Tomography reveals signs of an early stage of prostatitis, which is unattainable with other diagnostic methods. If abnormalities in the functioning of the prostate gland are suspected, MRI remains the preferred type of instrumental examination.
How long does treatment take
Stories of miraculous deliverance in a few days are nothing more than fairy tales. There is no quick way to cure prostatitis. After diagnosing the inflammation, you should set yourself up for long-term therapy and radical changes in eating habits and lifestyle. Only in this case will it be possible to defeat the disease.
Modern and effective methods of treating prostatitis have made it possible to shorten the treatment period. With an integrated approach, significant improvements can be achieved within 2-3 months.
Doctors have learned to cope with the consequences of prostatitis. The unique methods of therapy help to eliminate infertility, restore normal erection and increase sexual desire.
After achieving a stable remission, you will need to regularly take herbal medicines, attend physical therapy sessions for prevention and maintain men's health in other ways.
How is prostatitis treated?
There is no effective pill, after taking which all unpleasant symptoms will disappear. There is no such miracle cure among traditional medicine either. The best methods for treating prostatitis in men with proven effectiveness include an integrated approach: medication + physical therapy + non-traditional methods.
Official medicine offers conservative treatment. After completing the course, the unpleasant symptoms and negative manifestations of the disease disappear. At the second stage, the task is to eliminate the complications that have arisen.
Advanced non-invasive methods have increased the chances of a favorable outcome of the disease. Operative intervention is required in no more than 10-15% of cases.
With the help of drugs
Conservative therapy aimed at eliminating symptoms is carried out. The following groups of drugs are prescribed:

- NSAIDs- relief of inflammation, heat and fever. They have a mild analgesic effect. When prostatitis begins, short-term treatment with anti-inflammatory drugs and vitamins is necessary to keep the gland in a normal state. Medicines are available in suppositories, tablets and injections.
- antibiotics- designed to eliminate infectious or bacteriological inflammatory factors. The treatment scheme for prostatitis is prescribed after identifying the pathogen and testing its resistance to antibiotics. The course of treatment is 7-10 days. In severe cases, the therapy is extended to two weeks.
- Hormones- recommended if the usual course of treatment has not brought benefit, as well as in case of reduced sexual desire due to an advanced disease. Treatment with hormones at an early stage is prohibited. Medicines are taken under the strict control of a urologist.
- Symptomatic drugs— to eliminate pain, take acetylsalicylic acid tablets. Spasms are removed with an antispasmodic. An anesthetic block is indicated for persistent intense pain.
- vitaminsand medications to support prostate function. During the remission period, it is recommended to take drugs to normalize metabolism and improve blood supply to glandular tissues and juice production. Herbal medicines are prescribed for this purpose. A complex of vitamins and minerals is indicated to strengthen the immune system.
Self-medication is dangerous and does more harm than good. Before taking any of these drugs, you should consult a urologist.
Use of physical therapy
Prostatitis is characterized by extensive congestion in the pelvic area, which greatly complicates therapy. Taking drugs turns out to be ineffective, because the active components simply cannot be delivered from the blood vessels to the prostate gland.
In order to increase the effectiveness of drug therapy, immediately after relieving the exacerbation, physiotherapy is included in the course of treatment of prostatitis in men.
In addition to traditional electrophoresis, the following techniques are prescribed:
- UHF and microwave.
- Magnetotherapy.
- Mud treatment.
- Galvanizing.
- Ultraphonophoresis.
- Laser treatment.
- Heat therapy.
Most of the listed procedures are included in the complex of techniques used in balneotherapy. Contraindications for physiotherapy remain: acute period of inflammation, development of tumor tumors, individual intolerance of the patient.
Natural remedies
Modern methods of treating prostatitis increasingly combine official methods with alternative medicine. In ancient times, our ancestors treated prostatitis with herbal infusions, decoctions and bee products. The disease itself did not disappear, but the unpleasant symptoms were alleviated.
Some methods have survived to this day:
- Apitherapy— beekeeping products are used to eliminate inflammation and strengthen the immune system. Honey is a natural antibiotic. It is used to treat: death, propolis, wax, pollen, poison. Compresses and massage with honey, tinctures are made.
- Herbal collections- urological compounds are sold in pharmacies and you can prepare them yourself. Herbs treat urinary disorders, relieve inflammation and relieve pain. Some plants are good antiseptics. Decoctions and teas are prepared from the collections and added to compotes and tinctures.
In the old days, there were no hospitals and pharmacies. Diseases were treated with the help of the gifts of "mother nature". After prescribing a course of drugs, the urologist will definitely recommend one of the prescriptions of alternative medicine: herbal therapy or apitherapy.

Only an integrated approach to the fight against prostatitis will help to get rid of the disease once and for all. The success of treatment depends on early diagnosis and careful adherence to the urologist's recommendations.























